RESEARCH OVERVIEW
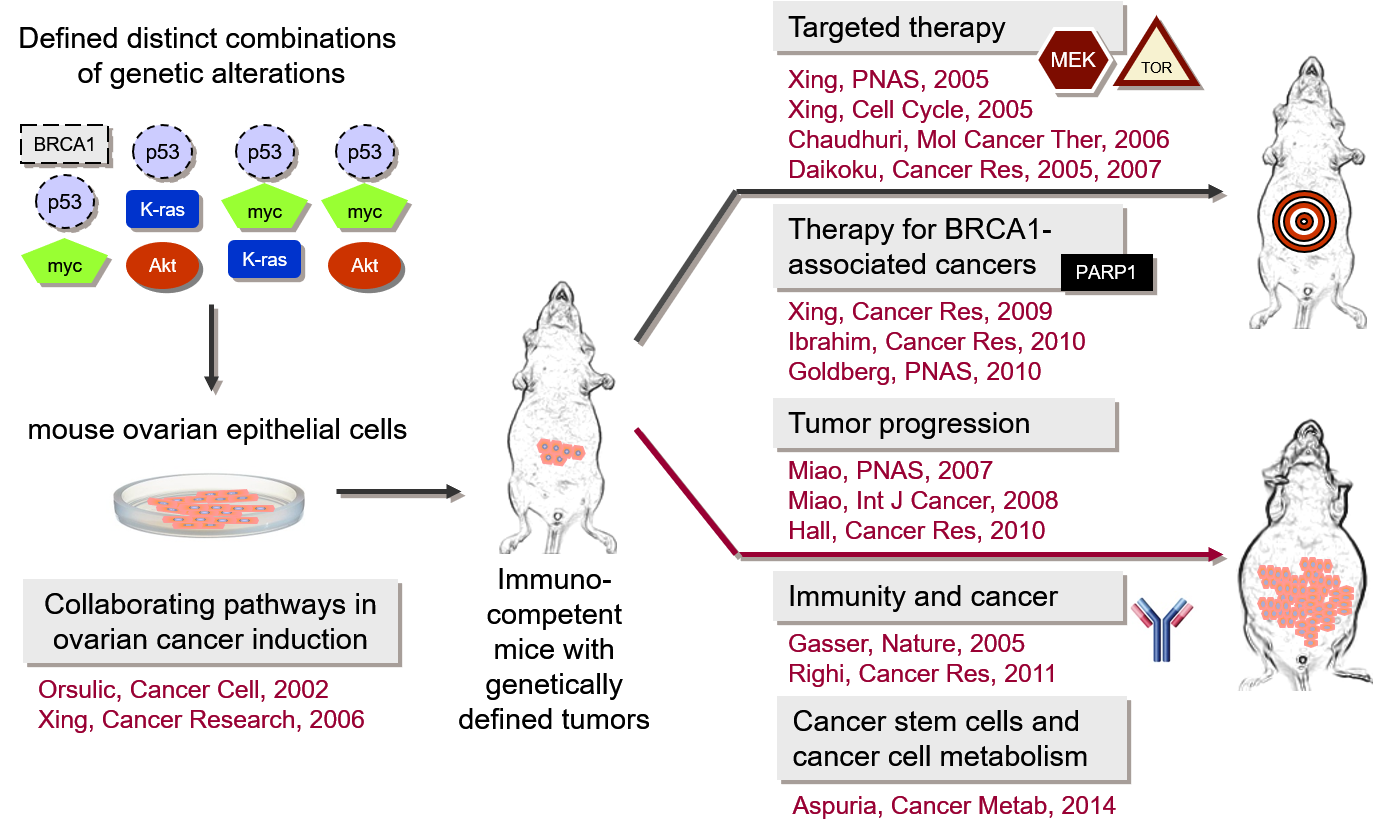
Our research focuses on the development of mouse models in which ovarian cancer can be induced and studied during its early stages of growth and metastatic progression. Our laboratory has generated multiple syngeneic mouse ovarian cancer cell lines with defined genetic alterations that recapitulate the development and pathophysiological manifestations of human ovarian cancer as well as the complexity of cancer-stroma interactions. We are using these models to determine the functional contributions of individual molecular pathways to cell transformation, immune response to cancer progression, recruitment of cancer-associated fibroblasts, and development of therapy resistance.
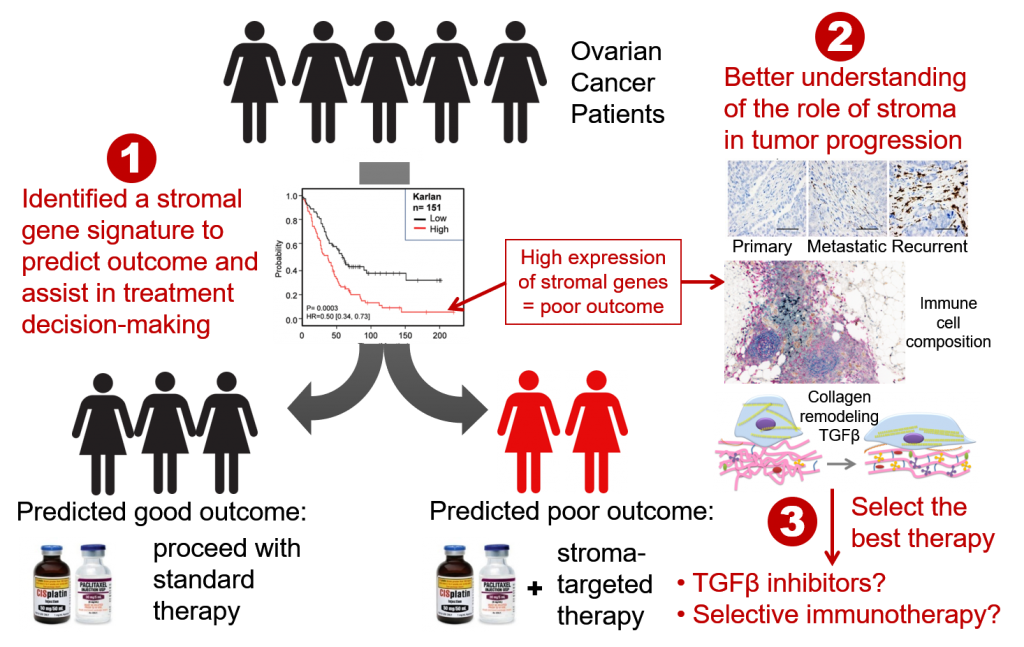
The Orsulic Lab is also working on the identification of discriminatory gene signatures that predict suboptimal cytoreduction, metastasis, recurrence, and poor survival in ovarian cancer patients. Our vision is to translate these signatures into clinically validated biomarkers for the identification of patients who are likely to experience early recurrence with standard surgery and chemotherapy and should be triaged to clinical trials at disease onset.
Other lines of investigation include:
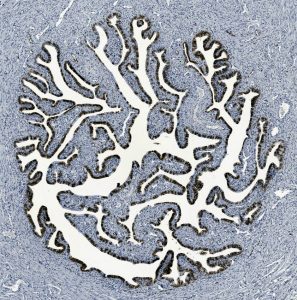
- Studies of the earliest stages of ovarian cancer cell attachment to the peritoneal surface
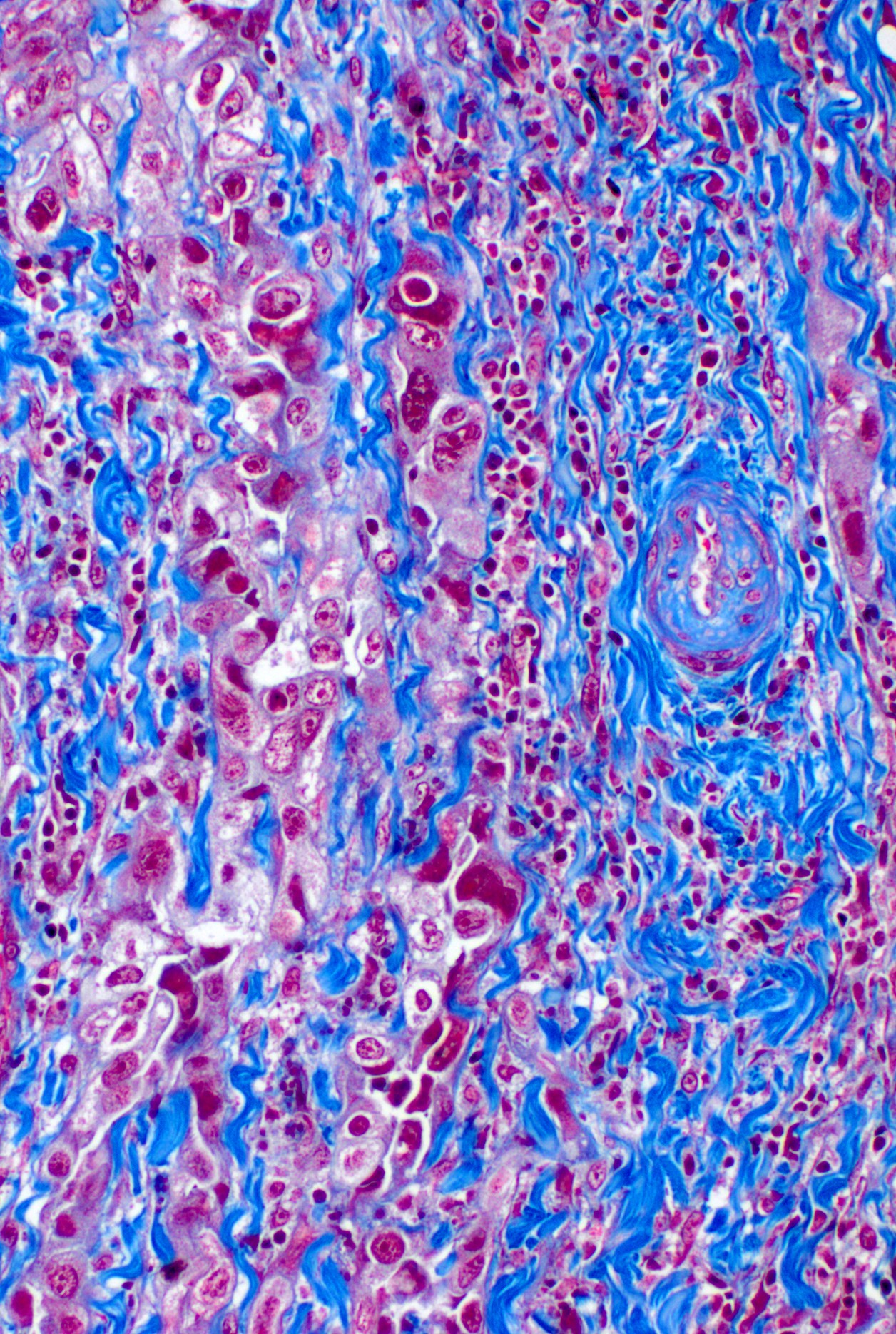
- Interactions between immune cells and cancer-associated fibroblasts/extracellular matrix
- Studies of the roles of BRCA1 and BRCA2 genes in ovarian cancer initiation
- Deep Learning-assisted digital image analyses for the identification of subvisual cellular and extracellular histomorphometric features that precede malignant transformation
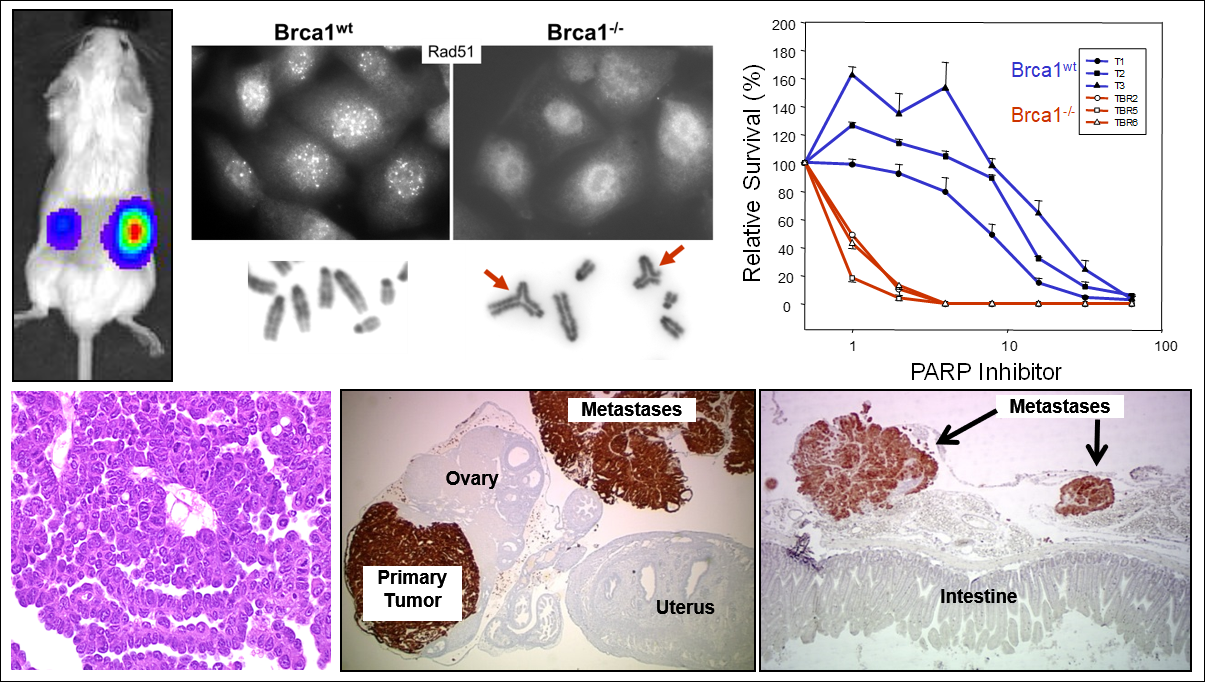
Our research has yielded several key insights into the molecular mechanisms of cancer. Our most significant contributions include: development of the first genetically defined mouse model of ovarian cancer; elucidation of the genetic events that are sufficient for the transformation of normal ovarian surface epithelial cells in the mouse; demonstration that specific molecular pathways collaborate in ovarian cancer induction and progression and that alternative signaling pathways play a role in resistance to targeted therapy; generation of the first syngeneic BRCA1-/- ovarian cancer cell lines; and identification of molecular biomarkers for individualized therapeutic strategies in ovarian cancer.

 The study of ovarian carcinogenesis has been limited by the lack of appropriate immunocompetent syngeneic mouse models that recapitulate genetic changes in human ovarian carcinoma. The Orsulic Laboratory has engineered multiple
The study of ovarian carcinogenesis has been limited by the lack of appropriate immunocompetent syngeneic mouse models that recapitulate genetic changes in human ovarian carcinoma. The Orsulic Laboratory has engineered multiple